Hypofractionation for Prostate Cancer: Where do we go next? - Juniper publishers
Journal of Trends in Technical and Scientific Research
Keywords: Hypofractionated radiotherapy; Toxicities, Acceleration; Protocols; Sensitivity; Tissues
Short Communication
Hypofractionated radiotherapy for localized prostate
cancer has recently been strongly recommended in evidence-based
guidelines jointly published by ASTRO, ASCO and AUA [1]. While it has
obvious advantages in cost and convenience, there remains a concern
about associated acute and late toxicities: Two randomized controlled
trials-HYPRO [2] and RTOG 0415 [3]-did identify a somewhat increased
risk of late toxicity, and several, CHHiP [4], PROFIT [5], HYPRO and Fox
Chase [6], all found increased risk of acute GI toxicity with
hypofractionation. These concerns are greater when
ultra-hypofractionation is used [1]. In order to reduce the acute and
late toxicities, our group at Grand River Hospital, Kitchener, Ontario,
back in 2006, started a Phase II trial [7] in which we stretched the
overall treatment time (OTT) to be the same as that in dose escalated
conventional radiotherapy, and showed that both acute and late
side-effects were very low with this intervention. Subsequently [8] have
shown in the PATRIOT trial that stretching the OTT is indeed
beneficial, when tested in a randomized fashion.
In this review, the radiobiological basis of
hypofractionation with stretching of OTT (which we call ‘Pure
Hypofractionation’, as it is free of the inherent acceleration seen in
most hypofractionation protocols) and how a large accurately designed
randomized trial could tell us whether we can improve the results of
hypofractionation for prostate cancer using pure hypofractionation, will
be discussed. The two radiobiologic hallmarks of prostate cancer are
‘high fractionation sensitivity’ and ‘slow repopulation’. The
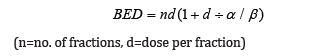
fractionation sensitivity is commonly expressed inversely as the
alpha/beta ratio; for most cancers as well as for ‘acute-reacting’
tissues like skin and mucosa, fractionation of a particular dose of
radiotherapy results in only a limited impairment of cell kill (low
fractionation sensitivity and high alpha/beta ratio), while for prostate
cancer and ‘late-reacting’ tissues like muscle & bone, the
cell-kill diminishes markedly withfractionation (high fractionation
sensitivity and low alpha/beta ratio). Therefore, when hypofractionation
is used, the total nominal dose required to ‘cure’ the prostate cancer
is lower than the total nominal dose used in conventionally fractionated
radiotherapy; this lower nominal dose produces a lower biologically
equivalent dose (BED) for the organs at risk (e.g. which have a higher
BED, as compared to that of prostate cancer of 1.5), as
This should result in a therapeutic advantage, with
lower acute and late side-effects with hypofractionation. Unfortunately,
this hope of reducing toxicity with hypofractionation has not been
borne out in the studies mentioned above. One reason for this could be
that hypofractionation protocols have an inherent acceleration in them,
as the overall treatment time (OTT) is shortened. Looking at the
following elaborate formula for BED, which takes the OTT also in
account, would explain why the acute side-effects of ‘accelerated’
hypofractionation would be worse:
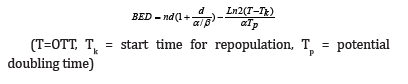
The OTT affects the repopulation during treatment,
which in turn affects cell-kill and acute toxicity. Thus, by
accelerating we increase the BED to rectal and bladder mucosa, leading
to not only the acute toxicity, but also the ‘consequential’ late
toxicity, which is particularly important in the rectum. The
corresponding increase in cell-kill to the prostate cancer is small,
given that the potential doubling time of prostate cancer is measured in
months (while that of rectal and bladder mucosa is measured in days).
Therefore, eliminating the inherent acceleration seen in most
hypofractionation protocols which have a shortened OTT wouldremove the
above therapeutic disadvantage. We believe that a
randomized clinical trial treating localized prostate cancer with
pure hypofractionation consisting of 6000cGy in 20 fractions
delivered over 8 weeks (every other working day) with the
standard arm being 7800cGy in 39 fractions over 8 weeks, would
help in clarifying whether this radiobiologic promise is borne out.
To Know More About Trends in Technical and
ScientificResearch Please click on:
https://juniperpublishers.com/ttsr/index.php
To Know More About Open Access
Journals Please click on:




Comments
Post a Comment